We envision a world where everyone has the tools and knowledge to live a balanced, healthy, and fulfilling life. By providing reliable resources, personalized programs, and community support, we aim to be a beacon of hope for those on their health journey.
Table of Contents
What is Non-Melanoma Skin Cancer?

non melanoma skin cancer
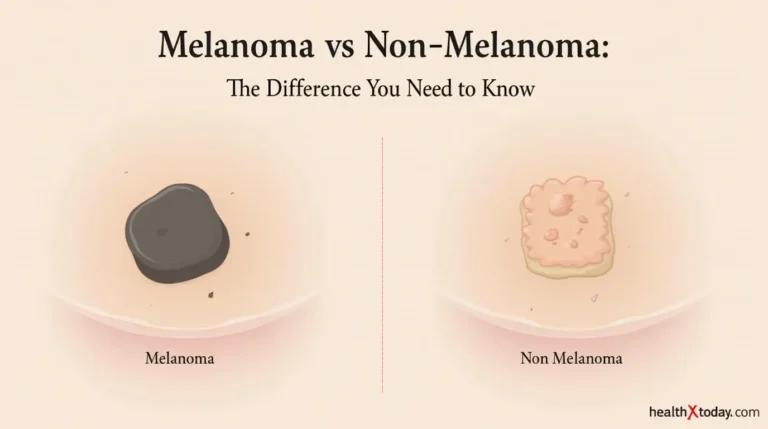
Non-melanoma skin cancer (NMSC) refers to a group of cancers that predominantly arise in the skin but are distinctly different from melanoma, which is considered a more aggressive and dangerous form of skin cancer. The most common types of non-melanoma skin cancer include basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). melanoma non melanoma; These cancers are generally associated with excessive exposure to ultraviolet (UV) radiation from the sun or tanning beds, leading to abnormalities in the skin’s basal and squamous cells, respectively.
Basal cell carcinoma, the most frequently diagnosed skin cancer, originates from the basal cells located in the lower epidermis. BCC often appears as pearly bumps, open sores, or red patches, typically on sun-exposed areas like the face, neck, and ears. This type of skin cancer tends to grow slowly and rarely metastasizes, making early detection and treatment vital for preventing extensive damage. Factors increasing the risk of developing BCC include fair skin, previous sunburns, and a history of skin cancer.
On the other hand, squamous cell carcinoma arises from the squamous cells that form the outer layer of the skin. SCC may appear as firm red nodules, scaly patches, or sores that crust or bleed. Although it is more likely than BCC to spread to other parts of the body if left untreated, SCC also has a favorable prognosis when detected early. Risk factors are similar to those for BCC, encompassing prolonged UV exposure, a compromised immune system, and a history of actinic keratosis.
In summary, understanding non-melanoma skin cancer is crucial for early diagnosis and effective management. By recognizing its types—BCC and SCC—as well as their characteristics and risk factors, individuals can take proactive measures towards prevention and early intervention.
Causes and Risk Factors
Non-melanoma skin cancer is primarily associated with several significant causes and risk factors that contribute to its development. One of the most substantial contributors is ultraviolet (UV) radiation exposure. This radiation comes predominantly from sunlight, with artificial sources like tanning beds also posing a risk. Prolonged and unprotected exposure to UV rays damages the DNA in skin cells, which can lead to mutations and, ultimately, cancer formation.
Skin type plays a crucial role in determining an individual’s susceptibility to non-melanoma skin cancer. People with fair skin, light hair, and light eyes are generally more at risk due to less melanin in their skin, which offers some protection against UV radiation. Conversely, individuals with darker skin tones have more natural protection, although they are not immune to skin cancer.
Familial history is another prominent risk factor. A genetic predisposition can significantly increase the likelihood of developing non-melanoma skin cancer, as certain hereditary conditions, such as xeroderma pigmentosum, heighten sensitivity to UV light. Additionally, individuals with a personal history of skin cancer are at an increased risk of developing further malignancies.
Weakened immune systems further compound these risks. Conditions such as HIV/AIDS or the use of immunosuppressive medications can hinder the body’s ability to fight off abnormal cell growth, making affected individuals more susceptible to cancerous changes in the skin. Environmental and lifestyle factors, such as exposure to certain chemicals, smoking, and a lack of regular skin checks, can also influence risk. It is essential for individuals to be aware of these risk factors to implement preventive measures and seek timely medical advice if necessary.
Symptoms and Early Signs

Non-melanoma skin cancer, which primarily includes basal cell carcinoma and squamous cell carcinoma, often presents with a range of symptoms and early warning signs. Recognizing these signs is crucial for timely intervention and effective treatment. The most common indicators include the appearance of new growths on the skin, which may emerge as smooth, shiny bumps or nodules, particularly in areas frequently exposed to sunlight such as the face, ears, neck, and hands.
Another hallmark of non-melanoma skin cancer is the presence of persistent sores that do not heal. These sores may bleed, crust over, or remain unhealed for several weeks or months, indicating a need for medical evaluation. Additionally, existing moles or spots can undergo changes in appearance; they may become larger, change color, or develop an irregular outline. Such alterations in pre-existing skin lesions are significant and warrant immediate attention.
In some cases, individuals may notice a textured or scaly patch on the skin that could be red, brown, or flesh-toned, often associated with squamous cell carcinoma. These patches may also sometimes itch or bleed. It is important to monitor any skin abnormalities and seek professional advice if any of these symptoms arise, as early detection can dramatically influence treatment outcomes and recovery chances. Regular skin checks, especially for those at higher risk factors include those with fair skin or a history of excessive sun exposure, can facilitate the identification of these early signs. It’s essential to prioritize skin health and consult with a healthcare provider promptly when any suspicious changes are observed.
Diagnosis of Non-Melanoma Skin Cancer
Diagnosing non-melanoma skin cancer involves a multi-faceted approach, primarily initiated through a thorough medical evaluation. First and foremost, healthcare professionals conduct a detailed physical examination of the patient’s skin. During this examination, the doctor will assess any abnormal growths or changes in existing moles, such as their size, shape, color, and texture. Identifying early symptoms is crucial, as timely diagnosis can significantly improve treatment outcomes.
Following the initial assessment, if non-melanoma skin cancer is suspected, a skin biopsy is often performed. This procedure entails removing a small sample of the suspicious skin area for laboratory analysis. There are several types of biopsies, including shave biopsies, punch biopsies, and excisional biopsies, each chosen based on the characteristics of the skin lesion. The histopathological examination of the biopsy specimen helps to determine the presence of cancerous cells and the specific type of non-melanoma skin cancer involved, whether it be basal cell carcinoma or squamous cell carcinoma.
In certain cases, imaging tests may also be employed, although they are not routinely used for initial diagnosis. These tests, such as ultrasound or CT scans, might be necessary if there is a concern that cancer has spread beyond the skin to nearby lymph nodes or other organs. Consulting a healthcare professional at the first signs of skin changes is of utmost importance, as they can recommend appropriate diagnostic procedures, ensuring that any potential non-melanoma skin cancer is identified and treated as early as possible. Early intervention can lead to more effective treatment options and a favorable prognosis for the patient.
Treatment Options Available

Treatment for non-melanoma skin cancer primarily depends on the type and stage of the disease. The most common treatment methods include surgical excision, cryotherapy, topical treatments, radiation therapy, and Mohs surgery, each offering specific advantages based on individual circumstances.
Surgical excision is one of the most frequently employed methods and involves removing the cancerous tissue along with a margin of healthy skin. This approach is particularly effective for basal cell carcinoma and squamous cell carcinoma. The surgeon aims to ensure complete removal to minimize the risk of recurrence. In many cases, this method provides excellent outcomes and is considered the standard treatment for localized tumors.
Cryotherapy, another viable option, utilizes extreme cold to freeze and destroy abnormal skin cells. This technique is often applied to superficial non-melanoma skin cancers and can be performed in an outpatient setting. Although less invasive, cryotherapy may not be suitable for all cases, especially those with deeper or larger lesions.
Topical treatments, including chemotherapy creams, are also utilized to treat certain types of non-melanoma skin cancer, particularly superficial basal cell carcinomas. Medications such as imiquimod or 5-fluorouracil are applied directly to the affected area, promoting the immune system’s ability to combat cancerous cells while minimizing damage to surrounding tissue.
Radiation therapy can serve as an alternative for individuals who cannot undergo surgery due to health complications or for cancers that are hard to reach. This method targets cancer cells with high-energy rays, effectively shrinking or eradicating tumors.
Lastly, Mohs surgery is a specialized surgical technique that involves the stepwise removal of cancerous skin, examining each layer microscopically until no further cancerous cells remain. This method is particularly beneficial for cancers in cosmetically sensitive areas, allowing for maximum tissue preservation while ensuring complete removal of the malignancy.
The selection of treatment options should always involve a thorough discussion between the patient and healthcare provider, considering factors such as tumor characteristics, patient preferences, and overall health.
Preventive Measures and Sun Safety
Preventing non-melanoma skin cancer is crucial, particularly in light of the increasing incidence rates associated with UV exposure. Adopting effective preventive measures can significantly reduce the risk of developing skin cancer. One of the primary strategies involves the daily application of a broad-spectrum sunscreen. It is vital to choose a sunscreen with an SPF of 30 or higher, ensuring protection against both UVA and UVB rays. Reapplication every two hours, and after swimming or sweating, is essential for maintaining its effectiveness.
In addition to sunscreen, wearing protective clothing serves as another layer of defense against harmful UV radiation. Long-sleeved shirts, pants, wide-brimmed hats, and UV-blocking sunglasses can provide significant protection while outdoors. It is also advisable to opt for clothing with an ultraviolet protection factor (UPF) rating, which indicates the level of UV protection provided by the fabric.
Seeking shade during peak sun hours, typically between 10 AM and 4 PM, is another crucial preventive measure. When planning outdoor activities, it is wise to take breaks under umbrellas, trees, or any form of shelter available to minimize direct sun exposure. Furthermore, the use of tanning beds should be strictly avoided, as they can contribute to an increased risk of developing non-melanoma skin cancer due to the concentrated UV exposure they provide.
Finally, regular skin checks are indispensable in catching any changes that may signify skin cancer early. Individuals should become familiar with their skin and monitor any unusual growths or changes in existing moles. Visiting a dermatologist for comprehensive skin examinations can greatly enhance the chances of early detection. By integrating these sun safety practices and consistent skin monitoring into daily routines, individuals can actively participate in lowering their risk of non-melanoma skin cancer.
Living with Non-Melanoma Skin Cancer
Receiving a diagnosis of non-melanoma skin cancer can have profound emotional and psychological effects on both patients and their families. Initially, individuals may experience a range of feelings including shock, anxiety, fear, and uncertainty about the future. It’s important to recognize that these reactions are entirely normal and may evolve as the reality of the situation sets in. The diagnosis can often disrupt daily routines and can create a ripple effect that impacts loved ones, leading them to experience similar emotional upheavals.
Effective coping strategies are essential to manage the emotional burden associated with non-melanoma skin cancer. Open communication with family members, friends, and support groups is a critical component of this process. Engaging in conversations about feelings, expectations, and fears can help alleviate feelings of isolation and foster a supportive environment. Additionally, educational resources that inform about non-melanoma skin cancer, treatment options, and survival outcomes can empower patients and their families, helping them to regain a sense of control over their circumstances.
Support resources play a vital role in the journey of individuals diagnosed with non-melanoma skin cancer. Many organizations offer counseling services, support groups, and informational workshops designed to guide patients through this challenging period. Connecting with others who have had similar experiences can provide comfort and valuable insights into navigating the treatment landscape.
Maintaining a positive outlook, while challenging, is crucial in coping with a non-melanoma skin cancer diagnosis. Techniques such as mindfulness, meditation, or even engaging in hobbies can serve as effective stress relievers. Building a strong support network comprising healthcare professionals, family, and community resources can significantly enhance emotional resilience during treatment. As the journey unfolds, drawing strength from these connections can make a considerable difference in one’s overall experience with non-melanoma skin cancer.
Latest Research and Advances in Treatment
The field of non-melanoma skin cancer treatment has seen significant advancements in recent years, driven by ongoing research and the development of innovative therapies. These new approaches aim to improve treatment outcomes while minimizing side effects and enhancing the overall patient experience. One of the most promising areas of research involves the use of targeted therapies that specifically attack cancer cells without harming healthy tissue. For instance, the recent approvals of topical immunotherapies, such as imiquimod and ingenol mebutate, have shown effectiveness in treating superficial basal cell carcinoma and actinic keratosis.
Alongside topical treatments, there is an increasing focus on systemic therapies, particularly for advanced cases of non-melanoma skin cancer. Research has highlighted the potential of immune checkpoint inhibitors, which work by enhancing the body’s immune response against cancer cells. Drugs such as pembrolizumab and nivolumab are currently being evaluated in numerous clinical trials, aiming to establish their effectiveness and safety for those with non-melanoma skin cancer that has spread beyond the skin.
Furthermore, ongoing clinical trials have explored the application of combination therapies, which involve using multiple treatment modalities to target the cancer comprehensively. These trials aim to determine the efficacy of combining surgical interventions with photodynamic therapy or radiation, particularly in cases where traditional approaches alone have yielded suboptimal results. non melanoma; The promise of personalized medicine is also emerging, as genetic profiling of tumors allows for tailored treatment strategies based on individual patient characteristics.
In conclusion, the landscape of treatment options for non-melanoma skin cancer is evolving rapidly. non melanoma; Advancements in targeted therapies, systemic treatments, and combination strategies provide hope for improved patient outcomes. non melanoma; Continued investment in research and clinical trials is vital, as emerging therapies hold the potential to reshape treatment protocols for non-melanoma skin cancer, ensuring that patients receive the most effective and personalized care possible.
References and Resources for Further Reading
For individuals seeking to deepen their understanding of non-melanoma skin cancer, a variety of reputable resources are available. non melanoma; Organizations dedicated to skin health provide valuable insights into prevention, diagnosis, and treatment. non melanoma; The American Academy of Dermatology (AAD) offers a comprehensive resource hub, detailing the latest research findings, patient education materials, and links to dermatologists who specialize in skin conditions. Their website can be accessed at www.aad.org.
The Skin Cancer Foundation is another prominent organization committed to skin cancer awareness and education. non melanoma; This foundation provides essential information on symptoms, risk factors, and treatment options specifically related to non-melanoma skin cancers. non melanoma; For more details, visit their website at www.skincancer.org. Their resources, including articles and brochures, are designed to inform the public about proactive measures that can reduce the risk of skin cancer.
Moreover, the National Cancer Institute offers a wealth of information on various types of skin cancer, including non-melanoma types such as basal cell carcinoma and squamous cell carcinoma. non melanoma; By navigating to www.cancer.gov, readers can access clinical trials, treatment protocols, and the latest statistics on skin cancer incidence and outcomes.
Support groups are also an invaluable resource for those affected by non-melanoma skin cancer. Organizations like Cancer Support Community provide emotional and practical support through group meetings, online forums, and educational workshops. non melanoma; Their website is available at www.cancersupportcommunity.org. These platforms quite effectively foster a sense of community and shared experiences among individuals navigating similar challenges.
In addition to these organizations, educational literature, such as books and articles written by experts in dermatology and oncology, can provide further insight into non-melanoma skin cancer. non melanoma; Engaging with this wealth of information can empower individuals to make informed decisions regarding their skin health.
Did You Try this tips ?
There are no reviews yet. Be the first one to write one.
blood work brain health cancer treatment climate health diabetes treatments digestive health disease management disease mapping exercise plan fitness tips hair care hair growth hair treatment headache treatment health apps health foods health insurance health secrets health tips healthy habits healthy recipes heart disease heart health home workouts immune boost immune foods keto delivery lifestyle diseases medicine innovation melanoma treatment mental health morning exercise natural remedies non melanoma nutritional advice raw nutrition skin cancer skin care skin health sleep exercise sleep technology telemedicine services viral threats walking benefits weight loss
non melanoma skin cancer: what you need to know now 1
Non-melanoma skin cancer (NMSC) refers to a group of cancers that predominantly arise in the skin but are distinctly different from melanoma, which is considered a more aggressive and dangerous form of skin cancer. The most common types of non-melanoma skin cancer include basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). melanoma non melanoma; These cancers are generally associated with excessive exposure to ultraviolet (UV) radiation from the sun or tanning beds, leading to abnormalities in the skin’s basal and squamous cells, respectively.