We envision a world where everyone has the tools and knowledge to live a balanced, healthy, and fulfilling life. By providing reliable resources, personalized programs, and community support, we aim to be a beacon of hope for those on their health journey.
Table of Contents
What is Chronic Kidney Disease (CKD)?

Chronic Kidney Disease (CKD) is a progressive medical condition characterized by a gradual decline in kidney function over an extended period. This decline impedes the kidneys’ ability to filter waste and excess fluid from the bloodstream, leading to a build-up of toxins and other potentially harmful substances. melanoma symptoms; The disease is classified into five distinct stages, with stage one being the mildest form and stage five representing kidney failure requiring dialysis or transplantation.
The glomerular filtration rate (GFR) is a critical metric used to gauge kidney function. It estimates how well the kidneys filter blood, with normal GFR values typically ranging from 90 to 120 mL/min. In CKD, the GFR decreases, correlating with the progression of the disease. For instance, a GFR below 60 mL/min for three months or more may indicate the presence of CKD. Understanding these numbers is vital not only for diagnosis but also for monitoring the disease’s progress and implementing timely interventions.
Diagnosing CKD involves evaluating various criteria, including the patient’s medical history, blood tests to measure serum creatinine levels, and urine tests to detect the presence of protein. The presence of persistent proteinuria, or protein in the urine, is a significant indicator of kidney damage. Additionally, factors such as blood pressure and the presence of diabetes are considered, as these conditions are among the leading causes of the disease. As CKD is often asymptomatic in its early stages, regular screening for at-risk populations is essential to identify individuals who may benefit from early intervention.
Causes and Risk Factors of CKD
Chronic Kidney Disease (CKD) is often a result of various underlying factors that damage the kidneys over time. The most significant causes include diabetes and hypertension, which account for over 70% of CKD cases. Diabetes, particularly Type 2, leads to high blood sugar levels that can damage the blood vessels and filters in the kidneys. This condition, known as diabetic nephropathy, is a critical concern among individuals with prolonged high glucose levels. Similarly, hypertension exerts excess pressure on the kidney’s blood vessels, leading to structural changes that diminish kidney function and can ultimately result in CKD.
Family history plays a vital role as well; those with a familial predisposition to kidney disease are more likely to develop CKD. Genetic factors can influence susceptibility to conditions that lead to kidney failure, highlighting the importance of monitoring kidney health in at-risk populations. Additionally, lifestyle factors such as poor diet and obesity are crucial risk contributors. Diets high in sodium, processed foods, and saturated fats can exacerbate the risks associated with diabetes and hypertension. Therefore, maintaining a balanced diet alongside regular physical activity is essential for reducing the likelihood of developing CKD.
Moreover, some less common causes of CKD can include autoimmune diseases like lupus nephritis, which occurs when the body’s immune system mistakenly attacks the kidneys. Certain medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs) taken over long periods, can lead to acute kidney injury and subsequent chronic issues if not carefully monitored. Identifying these causes and risk factors early can be instrumental in preventing or slowing the progression of Chronic Kidney Disease, reinforcing the need for routine health assessments and proactive management strategies.
Symptoms and Progression of CKD
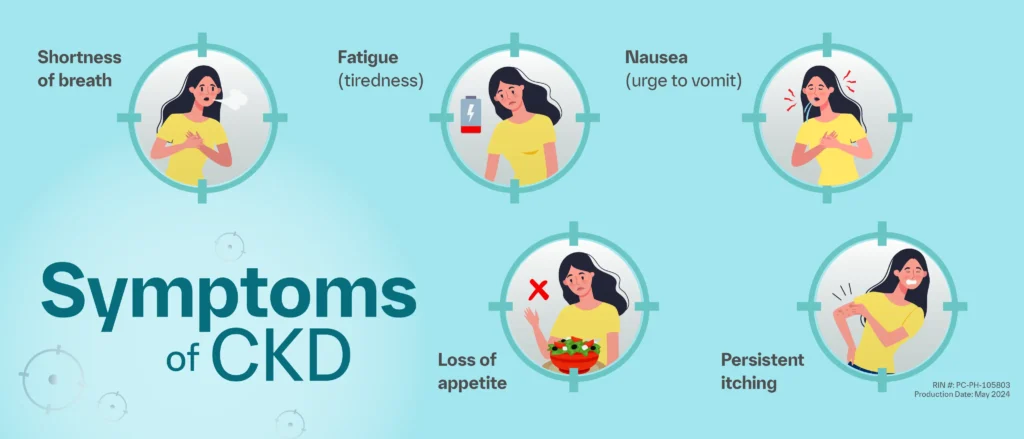
Chronic kidney disease (CKD) is defined as the gradual loss of kidney function over time. It is a serious condition that often goes unnoticed in its early stages due to subtle or absent symptoms. Many individuals may remain asymptomatic for years, which can delay diagnosis and treatment. As the disease progresses, however, a variety of symptoms may manifest, affecting patients’ overall health and quality of life.
In the early phases of CKD, some patients might experience mild symptoms such as fatigue, decreased appetite, or difficulty concentrating. These initial symptoms are often non-specific and can be attributed to numerous other conditions, making early detection challenging. As CKD advances, symptoms become more pronounced and may include swelling in the legs, ankles, or around the eyes due to fluid retention, and changes in urination patterns such as producing foamy urine or increased urgency. Patients may also experience persistent itching, nausea, and shortness of breath as a result of fluid build-up and waste accumulation in the blood.
The progression of chronic kidney disease is typically organized into five stages, each characterized by varying degrees of kidney function, as measured by glomerular filtration rate (GFR). In stage one, kidney function is still normal or mildly decreased, yet the individual is usually asymptomatic. As CKD progresses to stages two and three, signs and symptoms become more apparent, often inciting patients to seek medical advice. By stages four and five, patients face significantly reduced kidney function, leading to end-stage renal disease, which may require dialysis or kidney transplantation to sustain life.
Overall, the symptoms of CKD can have a profound impact on a patient’s daily activities and mental health. Monitoring kidney function and recognizing early signs of deterioration is critical for an effective management plan to enhance quality of life and slow disease progression.
Diagnosing Chronic Kidney Disease
Diagnosing Chronic Kidney Disease (CKD) involves several key methodologies aimed at assessing kidney function and identifying any underlying issues that may be contributing to renal impairment. The cornerstone of CKD diagnosis is blood testing, particularly measuring serum creatinine levels. Elevated serum creatinine is a strong indicator of compromised kidney function, reflecting the kidneys’ decreased ability to filter waste from the bloodstream. In conjunction with serum creatinine tests, the estimated glomerular filtration rate (eGFR) is calculated to provide a more comprehensive understanding of kidney performance.
Urine tests play an equally vital role in CKD diagnosis. A common method is a urinalysis, which can reveal proteinuria—excess protein in urine. This finding is significant, as the presence of protein can indicate early stages of kidney damage. Additionally, a more specific test is the urine albumin-to-creatinine ratio (UACR), which quantitatively assesses the level of albumin in the urine, providing important insights into kidney health.
Imaging studies, such as ultrasounds or CT scans, are also beneficial in diagnosing CKD. These non-invasive procedures allow healthcare providers to visualize the structure of the kidneys and identify any abnormalities, such as obstructions or size discrepancies, that could limit their function. Furthermore, in certain cases where additional detail is necessary, a kidney biopsy may be performed. This procedure involves obtaining a small sample of kidney tissue, enabling pathologists to evaluate the cause and extent of kidney damage at a cellular level.
Regular screenings for individuals at high risk for CKD, such as those with diabetes or hypertension, are paramount. Early detection through these methods can facilitate timely interventions, potentially halting or slowing the progression of the disease. It is crucial for healthcare providers to monitor kidney health continuously, ensuring that at-risk populations receive appropriate and proactive care.
Managing and Treating CKD

Effective management and treatment of chronic kidney disease (CKD) are crucial for slowing disease progression and maintaining overall health. This multi-faceted approach includes lifestyle modifications, medication management, and controlling underlying health conditions such as diabetes and hypertension, which are often associated with CKD. Lifestyle changes often denote the first line of defense in the management of kidney disease. Individuals are encouraged to adopt a balanced diet that is low in sodium, phosphorus, and potassium, thus enabling kidney function to be preserved. Regular physical activity is also recommended, as it helps to achieve a healthy weight, which can alleviate some of the strain on the kidneys.
In addition to lifestyle alterations, medications play an essential role in treating CKD. Anti-hypertensive medications, particularly ACE inhibitors or angiotensin receptor blockers (ARBs), can effectively manage blood pressure and have protective effects on kidney function. Additionally, controlling blood glucose levels is paramount for diabetic patients and may involve insulin or oral medications specifically designed for blood sugar control. Regular monitoring of kidney function through blood tests is essential to adjust these medications as necessary, ensuring they align with current health status.
For patients whose CKD progresses to end-stage kidney disease (ESKD), more advanced treatment options become essential. Dialysis, which includes hemodialysis and peritoneal dialysis, serves to artificially filter the blood when the kidneys are no longer able to do so. Hemodialysis is typically conducted in a clinical setting, while peritoneal dialysis can often be done at home. Furthermore, kidney transplantation presents an alternative for eligible patients, offering a potential return to a more functional state of health. It is vital for those considering transplant options to research compatible donors and understand the requisite post-operative care.
Dietary Considerations for CKD Patients
Chronic Kidney Disease (CKD) necessitates significant dietary modifications to help manage symptoms and slow disease progression. Nutrition plays a crucial role as it directly influences kidney function and overall health. Patients are often advised to adhere to specific dietary restrictions, particularly concerning the intake of potassium and phosphorus. Elevated levels of potassium can lead to serious heart problems, necessitating careful monitoring of foods rich in this mineral, such as bananas, oranges, and tomatoes. In contrast, phosphorus can accumulate in the blood and cause various complications, especially in later stages of CKD. Foods high in phosphorus, including nuts, seeds, and certain dairy products, should therefore be limited.
In addition to regulating potassium and phosphorus, it is vital for CKD patients to manage their protein intake. While protein is essential for the body’s functioning, excessive consumption can impose additional strain on already compromised kidneys. Patients may benefit from a tailored protein intake plan that balances nutritional needs and kidney health. Consulting with a healthcare provider or a registered dietitian can provide personalized guidance based on the individual’s stage of CKD, nutritional requirements, and lifestyle habits.
Hydration is another important aspect of dietary management for CKD patients. While it is crucial to stay adequately hydrated, individuals with CKD may need to monitor fluid intake and limit consumption based on their urine output and the existing health status. A dietitian can aid in creating a hydration strategy that aligns with medical advice and personal preferences.
Ultimately, maintaining a carefully structured diet under the supervision of a healthcare professional is essential for managing CKD effectively. By incorporating appropriate dietary adjustments, patients can potentially enhance their quality of life while minimizing the risks related to chronic kidney disease.
Living with Chronic Kidney Disease

Chronic Kidney Disease (CKD) is not only a physical health condition; it also brings significant emotional and psychological challenges for patients and their caregivers. The diagnosis of CKD can lead to feelings of anxiety, depression, and uncertainty about the future. The limitations imposed by the disease may affect everyday activities, which can complicate relationships and impact overall quality of life.
To cope with the emotional burden of CKD, patients and caregivers are encouraged to seek out support networks. Engaging with support groups can be particularly beneficial. These groups offer a platform for individuals to share their experiences and feelings, providing a sense of belonging and understanding. Patients can connect with others who genuinely understand the emotional turmoil associated with living with a chronic condition. These connections can help to alleviate feelings of isolation and provide a network of support during difficult times.
Moreover, it is essential to prioritize mental well-being alongside physical health. Mindfulness practices such as meditation and yoga can be effective strategies for managing stress and anxiety. Regular physical activity, within the limits advised by a healthcare provider, can also foster a sense of normalcy and improve mood. Furthermore, involving caregivers in these strategies is crucial, as they too can experience emotional strain when supporting a loved one with CKD.
Healthcare providers play a vital role in addressing the mental health aspects of CKD. Professional counseling or therapy should be considered when feelings of despair or hopelessness become overwhelming. Medical professionals can also provide resources and educational materials tailored to both patients and caregivers, empowering them with information and tools necessary to navigate the challenges of chronic kidney disease. Prioritizing emotional health is a crucial aspect of effectively managing CKD, ultimately leading to improved outcomes and resilience for both patients and their support systems.
Preventive Measures and Health Maintenance
Chronic Kidney Disease (CKD) can significantly impact an individual’s overall health, but understanding and implementing preventive measures can substantially reduce the risk of developing this condition. One of the most effective ways to combat CKD is through regular health check-ups. Routine evaluations enable early detection of any abnormalities in kidney function. Individuals should consult with healthcare professionals to determine an appropriate schedule for annual kidney function tests, especially if they have risk factors such as diabetes or hypertension.
Managing blood pressure and blood sugar levels is critical in preventing CKD. High blood pressure can damage the kidneys over time, while uncontrolled diabetes can lead to kidney complications. Individuals are encouraged to adhere to prescribed medication regimens and make lifestyle changes, such as reducing salt and sugar intake. Regular monitoring of these vital parameters can aid in understanding one’s health better and facilitate timely interventions when necessary.
In addition to medical management, adopting a healthy lifestyle plays a foundational role in kidney health. Engaging in regular physical activity, maintaining a balanced diet rich in fruits, vegetables, and whole grains, and avoiding excessive alcohol consumption can contribute to overall renal health. Furthermore, staying adequately hydrated helps kidneys function optimally. Education about kidney health is also essential; individuals should familiarize themselves with the risk factors and symptoms associated with CKD, fostering a proactive approach to their health.
Ultimately, a combination of regular monitoring, effective management of existing health conditions, and lifestyle modifications can significantly reduce the risk of developing Chronic Kidney Disease. These preventive steps contribute not only to kidney health but also to overall well-being, ensuring a healthier future.
Future Research and Developments in CKD
Chronic Kidney Disease (CKD) presents a global health challenge, prompting extensive research initiatives aimed at enhancing the understanding and management of this debilitating condition. One of the foremost areas of focus in current research involves the exploration of novel treatment options and pharmacological interventions that could potentially slow the progression of CKD. Clinical trials are being conducted to evaluate new medications that target specific pathways involved in kidney damage, including inflammation and oxidative stress, with the hope of preserving kidney function for longer periods.
In addition to pharmacotherapy, innovative approaches are being investigated, such as stem cell therapy and regenerative medicine. These therapies seek to repair or regenerate damaged kidney tissues, offering a promising avenue for patients with advanced stages of CKD. Researchers are also delving into the role of biomarkers in CKD, which can provide invaluable insights regarding disease progression and treatment efficacy. Identifying patients who are at high risk of rapid deterioration may lead to more personalized treatment strategies that are tailored to individual patient profiles.
Furthermore, the concept of personalized medicine is gaining traction within CKD research. By utilizing genetic, environmental, and lifestyle factors, healthcare providers can offer tailored therapeutic interventions that more effectively meet the needs of diverse patient populations. This individualized approach not only enhances treatment outcomes but also improves patient adherence and quality of life.
If successful, these advancements in research and treatment can significantly alter the landscape of CKD management, providing hope for millions affected worldwide. Ongoing studies will likely elucidate more effective therapies while opening new horizons for preventing and treating this chronic condition, marking an essential step forward in improving the prognosis for patients with CKD.
Did You Try this tips ?
There are no reviews yet. Be the first one to write one.
blood work brain health cancer treatment climate health diabetes treatments digestive health disease management disease mapping exercise plan fitness tips hair care hair growth hair treatment health foods health insurance health secrets health tips healthy habits healthy recipes heart disease heart health home workouts immune boost immune foods keto delivery keto recipes kidney disease lifestyle diseases medicine innovation melanoma treatment mental health morning exercise natural remedies non melanoma nutritional advice raw nutrition skin cancer skin care skin health sleep exercise sleep technology telemedicine services viral threats walking benefits weight loss
chronic kidney disease: you need to know now 101
Chronic Kidney Disease (CKD) is a progressive medical condition characterized by a gradual decline in kidney function over an extended period. This decline impedes the kidneys’ ability to filter waste and excess fluid from the bloodstream, leading to a build-up of toxins and other potentially harmful substances. melanoma symptoms; The disease is classified into five distinct stages, with stage one being the mildest form and stage five representing kidney failure requiring dialysis or transplantation.