We envision a world where everyone has the tools and knowledge to live a balanced, healthy, and fulfilling life. By providing reliable resources, personalized programs, and community support, we aim to be a beacon of hope for those on their health journey.
Table of Contents
What is Melanoma?

melanoma of skin cancer
Melanoma is a type of skin cancer that arises from melanocytes, which are specialized cells responsible for producing melanin, the pigment that gives color to our skin, hair, and eyes. Unlike other forms of skin cancer, such as basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), melanoma is more aggressive and has the potential to spread to other parts of the body. This malignant tumor typically presents as a change in an existing mole or the appearance of a new pigmented lesion that may have an irregular shape, Melanoma Cancer Warning Signs; varied coloration, and a diameter greater than 6 millimeters.
Several risk factors are associated with melanoma, including excessive sun exposure, particularly from ultraviolet (UV) radiation, a family history of skin cancer, and the presence of numerous moles or atypical moles. Individuals with fair skin, light hair, and blue or green eyes are also at a higher risk. Furthermore, certain genetic factors and a weakened immune system can increase susceptibility to this cancer. The incidence of melanoma has been rising in recent decades, making it an area of significant concern in public health.
The biological mechanisms underlying the development of melanoma involve mutations in the DNA of melanocytes, often triggered by UV radiation. These mutations can lead to unregulated cell growth and the formation of tumors. Inflammatory responses and the body’s failure to repair DNA damage also play crucial roles in melanoma progression. Understanding the distinct characteristics of melanoma compared to other types of skin cancer is essential for early detection and effective treatment, significantly influencing patient outcomes.
Types of Melanoma
Melanoma, recognized as one of the most aggressive forms of skin cancer, manifests in several distinct types, each with unique characteristics and implications for diagnosis and treatment. Understanding these types is crucial for early detection and effective management.
One of the most common varieties is superficial spreading melanoma, which typically appears as a flat or slightly elevated lesion with irregular borders and varied coloring. This type often occurs on areas exposed to the sun, such as the back, legs, and arms. It is frequently observed in younger individuals and is more prevalent among Caucasians, particularly those with fair skin.
Nodular melanoma represents another significant form and is distinguished by its raised appearance. This variety tends to grow vertically and can quickly metastasize to other areas of the body. Nodular melanoma is most commonly found on the trunk, head, and neck, affecting both men and women equally, with a higher incidence in older individuals.
Lentigo maligna melanoma typically arises from an existing lentigo, also known as age spots, and is often found on sun-damaged skin, particularly in older adults. It usually develops slowly over many years and can appear as a large, flat, dark area with irregular borders. This type is more frequent in individuals with a history of extensive sun exposure.
Lastly, acral lentiginous melanoma, though less common, is of particular concern as it primarily affects individuals with darker skin tones. It appears on non- sun-exposed areas such as the palms, soles, and under the nails. This type is more prevalent among African Americans and Asians, highlighting the importance of awareness across diverse populations.
In summary, recognizing the various types of melanoma aids in understanding the complexity and diversity of this potentially life-threatening skin cancer. Early detection and appropriate treatment are key to improving outcomes for all affected individuals.
Causes and Risk Factors
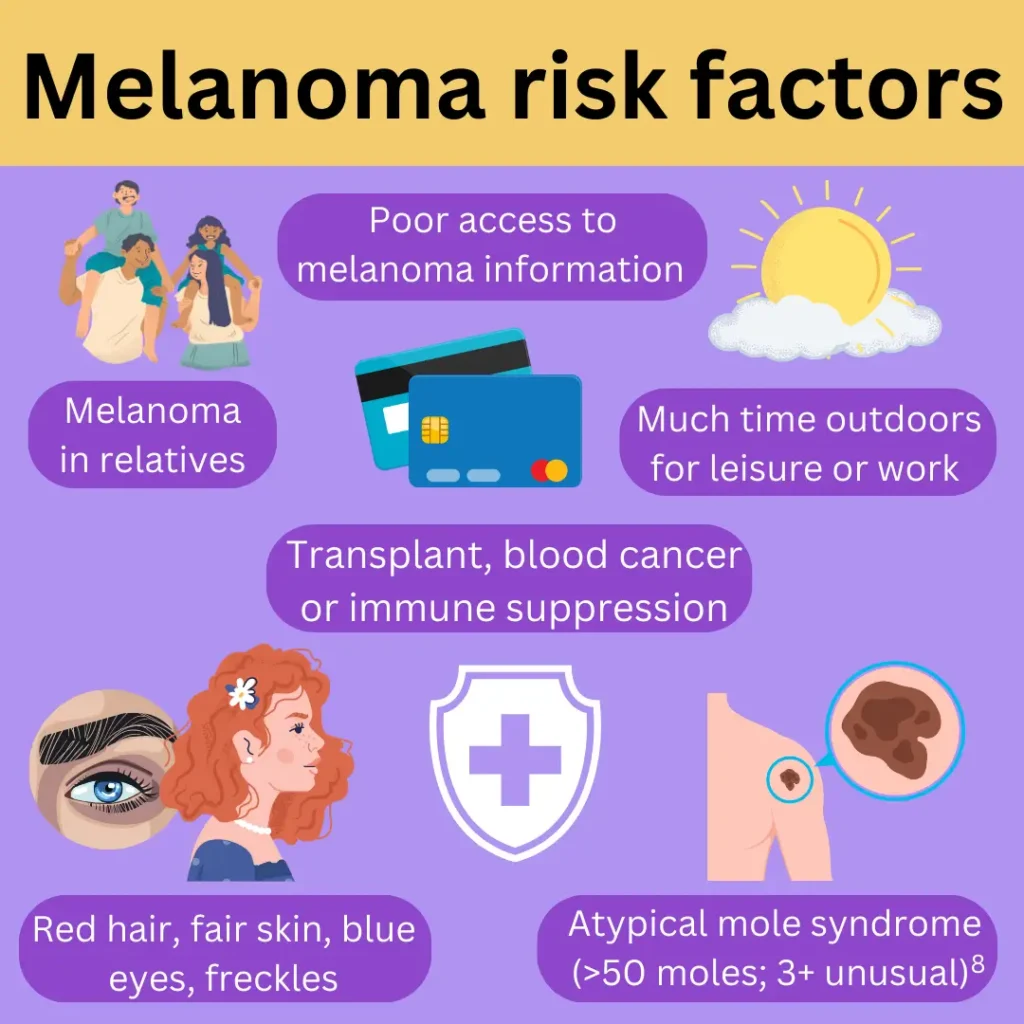
Melanoma, recognized as the most dangerous form of skin cancer, has its origins linked to a combination of genetic and environmental factors. Understanding the causes and risk factors associated with melanoma is crucial for effective prevention and early detection. One of the primary contributors to melanoma risk is exposure to ultraviolet (UV) radiation, which can arise from both natural sunlight and artificial tanning devices. It is well-established that intermittent intense sun exposure, particularly leading to sunburn, significantly elevates the likelihood of developing melanoma.
Genetic predispositions also play a pivotal role in melanoma risk. Family history has been demonstrated to increase vulnerability, suggesting that inherited genetic mutations may predispose certain individuals to this aggressive skin cancer. Notably, mutations in the CDKN2A gene are associated with a higher incidence of melanoma and related conditions. Skin type is another crucial factor; individuals with fair skin, light hair, or light eyes are at a greater risk due to reduced melanin levels that offer less natural protection against UV damage.
Age is a significant element to consider, as melanoma is more prevalent in older adults, with most cases diagnosed in individuals over the age of 50. However, it is important to acknowledge that the incidence among younger populations has been increasing in recent years, highlighting the need for vigilance across all age groups. Personal medical history is equally relevant; individuals with a previous diagnosis of melanoma or other skin cancers face heightened risk of recurrence or the development of new melanomas.
Recognizing these risk factors not only aids in understanding the etiology of melanoma but also serves as a foundation for preventive measures. Regular skin examinations and protective strategies against UV radiation exposure can lead to earlier detection, which is essential given the aggressive nature of melanoma.
Signs and Symptoms
Melanoma, a type of skin cancer arising from melanocytes, presents distinct signs and symptoms that warrant attention. Early detection significantly enhances treatment efficacy, making it essential for individuals to familiarize themselves with the characteristics of abnormal moles and skin changes. A widely recognized method for assessing moles is the ABCDE criteria, which provides a straightforward framework for individuals to identify potential melanomas.
The first criterion, Asymmetry, refers to a mole that lacks uniform shape; if a line were drawn down the middle, the two halves would not match. Next is Border, which emphasizes the need for attention to irregular, jagged, or blurred edges, indicating unusual growth. The Color criterion encourages individuals to look for variations in pigmentation within a mole that can appear black, brown, or multiple hues. Diameter is focused on size; moles larger than 6 millimeters (about the size of a pencil eraser) should be examined by a healthcare professional. Lastly, the Evolving criterion highlights any change in size, shape, or color over time, emphasizing that evolving moles can point to melanoma’s presence.
In addition to the ABCDE criteria, there are other warning signs that may suggest melanoma. These include the appearance of new moles after age 30, itchiness, tenderness, or pain at the site of a mole, and the emergence of lesions that ooze or bleed. Nevertheless, recognizing the signs and symptoms of melanoma is only part of effective prevention and early intervention.
Engaging in regular self-examinations is crucial for monitoring skin changes and understanding one’s baseline skin condition. In conjunction with self-exams, routine dermatological check-ups are essential for promptly identifying suspicious lesions and receiving professional guidance on skin health, thereby improving the chances of identifying melanoma in its earliest stages.
Diagnosis of Melanoma

Diagnosing melanoma, the most dangerous type of skin cancer, is a multi-step process that primarily involves thorough evaluations by healthcare professionals. The journey typically starts with a visual examination, where a dermatologist inspects the skin to identify any atypical moles or lesions that may indicate melanoma. During this examination, healthcare providers often utilize the ABCDE method: Asymmetry, Border irregularity, Color variation, Diameter larger than 6mm, and Evolving traits, which assists in detecting potential malignancies.
In addition to visual assessments, dermatoscopy plays a critical role in diagnosing melanoma. This specialized technique uses a dermatoscope, a handheld device, to provide a magnified and illuminated view of the skin, allowing dermatologists to differentiate between benign and malignant skin lesions more effectively. Dermatoscopy enhances the clarity of irregular moles, aiding in early detection, which is crucial for improving prognosis and treatment outcomes.
Should the visual examination and dermatoscopic findings raise suspicion, a biopsy is usually performed. This procedure involves removing a small tissue sample from the mole or lesion for microscopic evaluation. Biopsy techniques can vary, including shave biopsies, excisional biopsies, or incisional biopsies, depending on the size and location of the suspicious area. Pathologists then analyze the sample to determine whether malignant melanoma cells are present.
Early diagnosis remains paramount in the fight against melanoma. The earlier the skin cancer is detected and confirmed, the greater the chances of successful treatment and improved survival rates. Regular skin checks and awareness of changes in skin appearance can facilitate early diagnosis, underscoring the need for proactive skin health monitoring. With the advancement of diagnostic technologies, healthcare professionals are continuously improving their ability to detect melanoma at its earliest stages.
Stages of Melanoma
Melanoma is classified into distinct stages, each critical in determining the prognosis and treatment approaches for patients. The staging system primarily relies on the TNM classification, which assesses tumor size (T), involvement of lymph nodes (N), and the presence of metastasis (M). The stages range from 0 to IV, where stage 0 indicates localized melanoma and stage IV signifies advanced disease.
Stage 0, also known as melanoma in situ, is characterized by atypical cells present in the outermost layer of the skin, but which have not penetrated deeper tissues. At this point, the prognosis is exceptionally favorable, and complete surgical excision typically results in complete recovery.
Stage I indicates that the melanoma has grown but is still localized, with a maximum thickness of up to 2 millimeters and no lymph node involvement. At this stage, the prognosis remains positive, and surgical removal is generally sufficient for treatment.
Stage II melanoma is defined by greater thickness, with tumors ranging from 2 to 4 millimeters, or those that exhibit ulceration. Similar to stage I, there is no lymph node involvement; however, the risk of recurrence increases, making follow-up critical.
In stage III, the melanoma has spread to nearby lymph nodes, presenting a more complex scenario. The presence of cancer in these nodes can significantly affect treatment choices, often necessitating lymph node dissection and possibly adjuvant therapies.
Finally, stage IV is indicative of metastatic melanoma, where the cancer has spread beyond the original site to distant organs or tissues. This advanced stage poses the most significant treatment challenges, and a combination of systemic therapies, such as immunotherapy or targeted therapy, may be considered, depending on individual circumstances.
Overall, understanding these stages of melanoma is essential for patients and healthcare providers as they collaboratively develop effective treatment plans tailored to each patient’s specific condition.
Treatment Options for Melanoma

Melanoma, recognized as the most dangerous form of skin cancer, necessitates a comprehensive understanding of available treatment modalities. The choice of treatment often depends on the stage of the cancer, along with patient-specific factors such as overall health and preferences. The primary treatment option for melanoma is surgical removal, where the tumor and a margin of surrounding skin are excised. This approach is most effective in early stages when the melanoma is confined to the skin. Post-surgery, patients are often monitored closely to detect any recurrence.
In cases where melanoma has metastasized, immunotherapy becomes a pivotal option. melanoma cancer; This approach harnesses the body’s immune system to combat cancer cells, employing agents such as programmed cell death protein 1 (PD-1) inhibitors and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) inhibitors. Recent advancements have significantly improved survival rates with immunotherapy, although it can also induce adverse effects, including flu-like symptoms and skin reactions.
Targeted therapy is another promising avenue for treating melanoma, particularly for patients with specific genetic mutations such as BRAF. melanoma cancer; Medications that target these mutations aim to inhibit cancer cell growth. While targeted therapies have proven effective, they may come with side effects including fever, fatigue, and skin issues.
Chemotherapy and radiation therapy, while not typically first-line treatments for melanoma, may be utilized in certain advanced stages. melanoma cancer; Chemotherapy employs drugs to kill rapidly dividing cancer cells, but it usually comes with significant side effects such as nausea and hair loss. melanoma cancer; Radiation therapy aims to shrink or eliminate tumors and is often reserved for cases where surgery is not feasible or as an adjuvant treatment post-surgery.
Ultimately, the effectiveness of these treatments can vary greatly among individuals, emphasizing the necessity for personalized treatment plans. melanoma cancer; Physicians often consider factors such as the melanoma’s characteristics, the patient’s health, and potential treatment side effects when tailoring an approach. melanoma cancer;This individualized strategy aims to optimize treatment outcomes and improve the quality of life for those affected by melanoma.
Prevention and Self-Care Measures
Melanoma is the most dangerous form of skin cancer, and awareness of preventive measures and self-care strategies is crucial for reducing its risk. melanoma cancer; One of the most effective ways to protect yourself is by prioritizing sun protection. melanoma cancer; Exposure to ultraviolet (UV) radiation, whether from the sun or artificial sources like tanning beds, significantly increases the risk of developing melanoma. melanoma cancer; Therefore, applying a broad-spectrum sunscreen with a Sun Protection Factor (SPF) of at least 30 is essential, even on cloudy days or during winter. melanoma cancer; Reapplying sunscreen every two hours, or more frequently after swimming or sweating, can offer maximum protection.
Wearing protective clothing also plays a vital role in skin health maintenance. melanoma cancer; Opt for garments that cover the arms and legs, along with wide-brimmed hats to shield the face and neck from direct sunlight. Additionally, seeking shade whenever possible, especially during peak sunlight hours between 10 a.m. and 4 p.m., can further decrease UV exposure, helping to prevent melanoma.
Regular skin examinations are another key component of self-care. melanoma cancer; Individuals should become familiar with their skin and monitor any changes, such as new moles or alterations to existing ones. melanoma cancer; Adopting the ABCDE rule can aid in identifying concerning signs of melanoma. melanoma cancer; This includes assessing whether moles are Asymmetrical, have Irregular Borders, exhibit varied Colors, have a Diameter greater than 6mm, or show Evolution over time. melanoma cancer; Scheduling annual dermatological check-ups is highly advisable, particularly for those at higher risk due to a family history of skin cancer or previous instances of melanoma.
Incorporating these sun safety measures and remaining vigilant about skin changes allows individuals to take proactive steps in managing their skin health and reducing the likelihood of developing melanoma.
Living with and After Melanoma

Receiving a melanoma diagnosis can provoke a spectrum of emotional and psychological reactions, ranging from shock and fear to anxiety about the future. melanoma cancer; It is essential for those affected to acknowledge these feelings as part of the journey. melanoma cancer; Addressing the emotional impact involves finding effective coping strategies that empower patients and their families. melanoma cancer; Building a strong support system comprising family, friends, and healthcare professionals is vital in navigating this experience. melanoma cancer; Support groups, both in-person and online, can provide a safe space to share feelings and learn from others who have faced similar challenges.
Following treatment, the journey with melanoma continues, as ongoing monitoring is crucial. melanoma cancer; Regular follow-up appointments are essential to detect any signs of recurrence at an early stage. melanoma cancer; Patients are typically advised to schedule periodic skin examinations with their dermatologist and may undergo imaging or blood tests depending on their specific case. melanoma cancer; This vigilant approach not only aids in the early detection of potential recurrences but also reinforces the importance of self-examinations and awareness of changes in the skin.
Lifestyle adjustments can play a significant role in enhancing overall well-being post-melanoma. melanoma cancer; Many survivors choose to implement healthier habits, which may include adopting a balanced diet, engaging in regular physical activity, and staying vigilant about sun protection. melanoma cancer; This proactive approach supports not only physical health but also mental resilience, contributing to a more positive outlook on life after treatment. melanoma cancer; Resources available for melanoma survivors, including educational materials, counseling services, and wellness programs, are designed to help individuals and their families adjust to life after melanoma. melanoma cancer; Employing these resources can facilitate a smoother transition into survivorship, effectively empowering individuals to take charge of their health moving forward.
Did You Try this tips ?
There are no reviews yet. Be the first one to write one.
blood work brain health cancer treatment climate health diabetes treatments digestive health disease management disease mapping exercise plan fitness tips hair care hair growth hair treatment health apps health foods health insurance health tips healthy habits healthy recipes heart disease home workouts immune boost immune foods keto plan keto recipes kidney disease lifestyle diseases meal delivery medicine innovation melanoma treatment mental health morning exercise natural remedies non melanoma nutritional advice nutrition assistance raw nutrition skin cancer skin care skin health sleep exercise sleep technology telemedicine services viral threats weight loss
melanoma of skin cancer get info to know1 now
Melanoma is a type of skin cancer that arises from melanocytes, which are specialized cells responsible for producing melanin, the pigment that gives color to our skin, hair, and eyes. Unlike other forms of skin cancer, such as basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), melanoma is more aggressive and has the potential to spread to other parts of the body. This malignant tumor typically presents as a change in an existing mole or the appearance of a new pigmented lesion that may have an irregular shape, Melanoma Cancer Warning Signs; varied coloration, and a diameter greater than 6 millimeters.