Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Tuberculosis (TB) is an infectious disease that primarily affects the lungs but can also impact other parts of the body. Caused by the bacterium Mycobacterium tuberculosis, TB has been a significant public health issue for centuries. Historically, tuberculosis was often referred to as “consumption” due to the severe weight loss and wasting it caused in its victims. Despite advancements in medical science, TB remains a global health crisis, particularly in developing countries where healthcare resources are limited.
According to the World Health Organization (WHO), approximately ten million people developed TB in 2020, and around 1.5 million people died from the disease, making it one of the leading causes of death worldwide. This high prevalence underscores the persistent challenge TB poses to public health systems despite the availability of advanced diagnostic tools and effective treatments.
Tuberculosis manifests in two main forms: latent TB and active TB. Latent TB occurs when an individual is infected with Mycobacterium tuberculosis, but the bacteria remain dormant within the body and do not cause symptoms. Individuals with latent TB are not contagious but are at risk of developing active TB if their immune system becomes compromised. Active TB, on the other hand, is characterized by the presence of symptoms such as a persistent cough, chest pain, and fatigue. Unlike latent TB, individuals with active TB are contagious and can spread the bacteria to others through respiratory droplets.
Understanding the different types of tuberculosis is crucial for effective public health interventions aimed at controlling and eventually eradicating the disease. Efforts to combat TB include widespread screening, vaccination programs, and the development of comprehensive treatment plans for those infected.
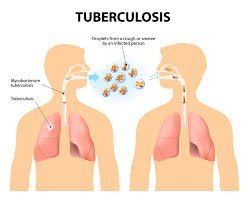
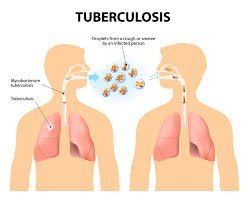
Tuberculosis (TB) is primarily caused by the bacterium Mycobacterium tuberculosis. This pathogenic organism is uniquely adapted to thrive in the human body, typically affecting the lungs but also capable of infecting other parts of the body. The hallmark of TB’s transmission lies in its airborne nature, making it a highly infectious and widespread disease. When individuals with active pulmonary TB expel bacteria into the air through actions such as coughing, sneezing, or even speaking, these bacteria are encapsulated in tiny droplets that can be inhaled by others, leading to new infections.
Once inhaled, the bacteria can settle in the lungs, where the immune system’s response determines whether the TB will remain latent or progress to active disease. It is crucial to understand the distinction between latent and active TB to comprehend the dynamics of its spread. Latent TB means the bacteria remain in an inactive state within the body, causing no symptoms and not being contagious. However, active TB signifies a proliferative phase where the person exhibits symptoms and can transmit the disease to others.
Several factors elevate the risk of TB transmission and contraction. Foremost among them is close and prolonged contact with an individual who has active TB, particularly in poorly ventilated or crowded environments. Immunocompromised conditions, such as HIV/AIDS, diabetes, or undergoing immunosuppressive therapy, significantly heighten one’s susceptibility to TB. Malnutrition, substance abuse, and living in or traveling to areas with high TB prevalence further compound the risk.
Mitigating the transmission of TB involves a multi-faceted approach, including prompt diagnosis and appropriate treatment of active TB cases, vaccination with the Bacillus Calmette-Guérin (BCG) vaccine, and sustained public health measures aimed at reducing both societal and individual risk factors. Balancing these strategies is pivotal to controlling and eventually eradicating tuberculosis as a global health threat.
Tuberculosis (TB) manifests through a range of symptoms, varying significantly depending on the stage of the disease. In its early phase, known as latent TB infection, individuals carry the TB bacteria but remain asymptomatic. This stage is typically non-infectious; however, it holds the risk of transitioning to active TB disease if not properly managed.
The progression to active TB disease introduces a series of more pronounced symptoms. The hallmark of active TB is a persistent cough lasting three weeks or more. This cough may be accompanied by hemoptysis, characterized by coughing up blood or sputum. Patients often experience systemic symptoms including fever, night sweats, and considerable weight loss. Fatigue and malaise are also common, contributing to the overall debilitating nature of the disease.
TB primarily affects the lungs (pulmonary TB), where it incites severe respiratory symptoms. Pulmonary TB can significantly impair lung function, leading to chest pain and breathlessness. However, Mycobacterium tuberculosis, the causative agent, can also target other bodily regions, resulting in extrapulmonary TB. The symptoms of extrapulmonary TB are variable and depend on the organ involved. For instance, TB of the spine (Pott’s disease) might cause back pain, whereas TB meningitis could present with headaches, neurological impairments, and even seizures.
Understanding the distinction between latent and active TB is crucial. Latent TB, while dormant, can reactivate especially in individuals with compromised immune systems, such as those with HIV or diabetes.
Diagnosing tuberculosis (TB) requires a comprehensive approach involving several diagnostic methods. Among the most common and initial procedures is the Tuberculin Skin Test (TST). During this test, a small amount of tuberculin purified protein derivative is injected just under the skin of the forearm. If there is a significant swelling at the site of the injection after 48-72 hours, it indicates a possible TB infection. While TST is beneficial due to its simplicity and cost-effectiveness, it has limitations; a positive result does not necessarily differentiate between active TB disease and latent TB infection and can also produce false positives in individuals previously vaccinated with Bacille Calmette-Guérin (BCG).
The Interferon-Gamma Release Assays (IGRAs) are blood tests that measure the immune response to TB bacteria. Unlike TST, IGRAs are not affected by prior BCG vaccination, making them more specific in certain populations. Two major types of IGRAs are the QuantiFERON-TB Gold In-Tube test and the T-SPOT.TB test. These tests offer benefits in terms of higher specificity and faster results, generally within 24 hours. However, like TST, IGRAs cannot differentiate between latent TB infection and active TB disease.
Chest X-rays are another critical tool in diagnosing TB. They can reveal changes in the lungs that suggest TB, such as lesions, nodules, and cavitations.
Sputum tests are paramount for a definitive TB diagnosis, especially for pulmonary TB. Sputum culture, more specifically, allows for not just identification but also for testing drug susceptibility. This method is highly specific, but it requires a longer period, often weeks, to obtain results.
Each diagnostic method for TB has its advantages and limitations. A combination of tests is often employed to achieve a comprehensive and accurate diagnosis, enabling appropriate and effective treatment plans. Improving diagnostic accuracy remains a critical goal in the global fight against tuberculosis.
Tuberculosis (TB) treatment primarily involves the administration of multiple antibiotics over an extended period, typically ranging from six to nine months. The standard treatment regimen for active TB includes a combination of first-line antitubercular drugs such as isoniazid, rifampin, pyrazinamide, and ethambutol. This multi-drug approach is critical to effectively eliminate Mycobacterium tuberculosis and to prevent the development of drug-resistant strains.
Adherence to the prescribed treatment plan is imperative for successful recovery. Patients must follow their medication schedule diligently to avoid incomplete treatment, which can lead to the recurrence of the disease and increase the risk of developing multi-drug-resistant TB (MDR-TB). MDR-TTB is a form of tuberculosis that does not respond to at least isoniazid and rifampin, the two most potent TB drugs, necessitating even longer and more complex treatment plans involving second-line drugs that often have more severe side effects.
The management of drug-resistant TB strains remains a significant challenge. It requires tailored treatment strategies that may include newer drugs such as bedaquiline and delamanid. Given the complexity and potential adverse reactions, treatment plans for MDR-TB and extensively drug-resistant TB (XDR-TB) should be closely monitored by healthcare professionals. Frequent consultations and regular check-ups help manage side effects and ensure the efficacy of the treatment regimen.
Directly Observed Therapy (DOT) plays a crucial role in the management of TB by ensuring that patients adhere to their treatment plans. Under DOT, healthcare workers directly observe patients as they take their medications, which significantly increases cure rates and reduces the spread of TB. It is especially effective in low-resource settings where healthcare access and patient compliance may be challenging.
In conclusion, effective tuberculosis management requires a thorough understanding of the standard treatment protocols, strict adherence to medication schedules, and appropriate measures to tackle drug-resistant strains.
Preventing tuberculosis (TB) is paramount to controlling its spread and minimizing its impact on public health. One of the most effective preventive measures is vaccination, specifically the Bacillus Calmette-Guérin (BCG) vaccine. The BCG vaccine is generally administered to infants in countries with high TB prevalence and has shown efficacy in preventing severe forms of TB in children. However, its effectiveness varies geographically and among different age groups, underscoring the need for additional preventive strategies.
Improving living conditions is another crucial strategy in the fight against TB. Overcrowded and poorly ventilated living spaces can facilitate the transmission of Mycobacterium tuberculosis, the bacterium responsible for TB. Ensuring adequate ventilation, reducing overcrowding, and maintaining good hygiene can significantly reduce the spread of the disease.
Reducing stigma associated with TB is equally important. Individuals with TB often face social ostracization, which can hinder their willingness to seek diagnosis and treatment. Public education campaigns that dispel myths and inform the public about the nature of TB can mitigate stigmatization. Health professionals also play a vital role in fostering a supportive environment for TB patients, encouraging early detection and compliance with treatment regimens.
Public health initiatives and community engagement are indispensable in TB prevention. Active case finding, regular screening programs, and health education significantly contribute to early detection and treatment. Early diagnosis is key; it not only improves patient outcomes but also curtails the spread of TB within communities. Initiatives like directly observed treatment, short-course (DOTS), enhance treatment adherence and have been instrumental in reducing TB cases globally.
Ultimately, preventing tuberculosis requires a multifaceted approach that includes vaccination, improved living conditions, stigma reduction, and proactive public health measures. By adopting these strategies collectively, we can make significant strides towards eradicating TB.
Tuberculosis (TB) remains one of the most significant global health challenges, affecting millions of lives each year. As per the World Health Organization (WHO), TB ranks among the top 10 causes of death worldwide, illustrating its widespread impact. In 2021 alone, there were an estimated 10 million new TB cases globally, with 1.5 million resulting in fatalities. These staggering numbers underline the urgent need for continuous efforts to combat this persistent disease.
TB’s prevalence is notably higher in low- to middle-income countries, where socioeconomic factors play a critical role. Countries like India, Indonesia, China, the Philippines, and Pakistan represent roughly half of the world’s TB burden. Poverty exacerbates the situation by hindering timely diagnosis and effective treatment, thereby perpetuating the disease cycle.
The socio-economic impact of TB is profound, often disrupting communities and imposing a heavy economic burden.
Various international organizations are at the forefront of the fight against TB, working to reduce its global impact. The WHO End TB Strategy aims to cut TB deaths by 90% and reduce new cases by 80% between 2015 and 2030. Complementing these efforts, organizations such as the Stop TB Partnership and TB Alliance are striving to accelerate research, development, and access to better diagnostics, treatments, and vaccines. Their collaborative efforts are essential in making significant strides toward TB control and eventual eradication.
International cooperation is crucial in addressing the multifaceted nature of TB. Tailored strategies that consider local socio-economic contexts, combined with sustained financial and political commitment, are vital components of a comprehensive approach to mitigating this global health crisis. With continued dedication and innovation, it is possible to make meaningful progress in reducing the global burden of tuberculosis.
The landscape of tuberculosis (TB) research continues to evolve as scientists and healthcare professionals strive to develop more effective diagnostic tools, vaccines, and treatments. Ongoing research focuses on various fronts, including the exploration of novel biomarkers for quicker and more accurate diagnosis. Recent advances in molecular diagnostics, such as GeneXpert and other rapid testing platforms, have shown promise in identifying TB infection more swiftly than traditional methods. These innovations are crucial for early detection and prompt treatment, which significantly improve patient outcomes.
In addition to diagnostic tools, TB vaccine development remains a top priority. The Bacillus Calmette-Guérin (BCG) vaccine has been the only vaccine available for nearly a century, offering limited protection. Researchers are now investigating several new vaccine candidates, aiming to provide broader and more durable immunity. The M72/AS01E candidate, for instance, has shown promising results in recent clinical trials, highlighting the potential for more effective prevention strategies in the near future.
Emerging technologies, such as artificial intelligence (AI) and machine learning, are also playing a pivotal role in TB research. These technologies can analyze vast datasets to predict TB trends, optimize treatment regimens, and identify potential drug resistance patterns. Additionally, advancements in genome-editing tools like CRISPR hold potential for developing targeted therapies that could revolutionize TB treatment.
Global collaboration is paramount in tackling TB. Collaborative efforts can accelerate the development of new tools and strategies, ultimately reducing the global TB burden.
However, researchers face significant challenges, including drug resistance, limited resources, and logistical hurdles in conducting large-scale clinical trials. Securing sustained investment in TB research is essential to address these challenges and ensure continuous progress. By prioritizing TB research and fostering global collaboration, the scientific community can make significant strides towards eradicating this disease.