We envision a world where everyone has the tools and knowledge to live a balanced, healthy, and fulfilling life. By providing reliable resources, personalized programs, and community support, we aim to be a beacon of hope for those on their health journey.
Table of Contents
What is Melanoma?

melanoma skin cancer
Melanoma is a serious form of skin cancer that originates in melanocytes, the cells responsible for producing the pigment melanin, which gives color to the skin. This type of cancer is notably more aggressive than other forms of skin cancer, such as basal cell carcinoma or squamous cell carcinoma, primarily due to its ability to metastasize. Melanoma can arise from existing moles or appear as new pigmented lesions on the skin. Its distinctive characteristics and behavior necessitate careful monitoring and understanding.
One of the fundamental aspects of melanoma is its classification into stages, which is critical in determining treatment options and predicting outcomes. Health Insurance; The staging ranges from stage 0, indicating melanoma in situ, to stage IV, which denotes advanced metastatic melanoma. Stage 0 melanoma is localized and has not penetrated deeper layers of the skin, while stage IV signifies that the cancer has spread to distant parts of the body, such as the lungs or liver. Early stages typically present with a better prognosis, highlighting the importance of early detection and intervention.
Symptoms of melanoma can vary widely. The significant warning signs include changes in the size, shape, or color of moles or the emergence of new pigmented spots. These changes may present as asymmetry, irregular borders, multiple colors, a diameter larger than a pencil eraser, or any evolution over time—collectively referred to as the ABCDE criteria. Prompt recognition of these signs can lead to critical early diagnosis, enabling successful treatment outcomes. Understanding the nature and development of melanoma is vital, as it positions patients to recognize symptoms that may warrant further examination by healthcare professionals, thus facilitating timely medical intervention.
Symptoms of Melanoma
Melanoma, a serious form of skin cancer, often manifests through distinct symptoms that warrant careful observation. The early detection of melanoma is critical, as it significantly improves treatment outcomes. One of the primary tools used to identify potential melanomas is the ABCDE rule, which provides guidelines based on specific characteristics of moles and skin lesions.
The first component, Asymmetry, refers to moles or spots that do not have matching halves. When one side differs in shape or size from the other, this discrepancy can be a warning sign. The second characteristic, Border, highlights the irregular nature of the edges of a mole. While benign moles often have smooth, even borders, a melanoma may exhibit uneven, scalloped, or notched edges. The third factor, Color, indicates that melanomas may display a variety of hues, including shades of brown, black, red, white, or blue, contrasting with the typically uniform color of non-cancerous moles.
Diameter is the fourth element of the ABCDE rule. A mole larger than 6 millimeters, roughly the size of a pencil eraser, should be evaluated for possible melanoma. The final component, Evolving, signifies any change in a mole regarding size, shape, color, or elevation. Any alterations in existing moles, or the appearance of new growths, should alert individuals to seek a medical consultation.
In addition to the ABCDE criteria, other symptoms may suggest melanoma. These include sores that do not heal, persistent itching or tenderness, and any red or painful lesions. It is vital for individuals to regularly monitor their skin for changes and consult a healthcare professional if any concerning symptoms arise. Early detection is key in effectively combating melanoma and improving patient outcomes.
Risk Factors for Melanoma
Melanoma, a serious form of skin cancer, is influenced by various risk factors that can significantly impact an individual’s likelihood of developing the disease. Understanding these factors is crucial for effective prevention and early detection. One of the primary risk factors is genetic predisposition. Individuals with a family history of melanoma are at a higher risk, as genetics play a key role in skin cancer susceptibility. Specific gene mutations, such as those in the CDKN2A gene, are associated with an increased likelihood of melanoma in families.
Environmental exposures are equally significant, particularly ultraviolet (UV) radiation from sunlight and artificial sources like tanning beds. Prolonged exposure to UV rays can damage the DNA in skin cells, leading to mutations that may result in melanoma. Thus, individuals who frequently sunbathe or use tanning beds are at an elevated risk. Regions with higher sun exposure also contribute to increased melanoma cases, underscoring the importance of sun protection in vulnerable populations.
Skin type is a critical risk factor as well. Those with fair skin, light-colored eyes, and red or blond hair are particularly susceptible to melanoma. The pigmentation in darker skin provides some natural protection against UV radiation; however, malignancies can still occur in individuals of all skin types. Moreover, a personal history of skin cancer, including non-melanoma forms like basal cell carcinoma or squamous cell carcinoma, can increase the risk of developing melanoma. Frequent skin examinations and awareness of changes in existing moles or new growths can aid in early diagnosis.
In conclusion, recognizing the various risk factors for melanoma, including genetic predispositions, environmental influences, and individual characteristics, is essential for prevention. By understanding these risks, individuals can adopt proactive measures to protect their skin and reduce the likelihood of developing this serious form of skin cancer.
Diagnosis of Melanoma
The diagnosis of melanoma, a serious form of skin cancer, involves a systematic approach that includes thorough physical examinations, specialized imaging techniques, and biopsy procedures. Dermatologists, specialists in skin conditions, play a crucial role in identifying melanoma at its initial stages, thereby increasing the chances of effective treatment. Regular skin checks, whether self-examinations or professional assessments, are vital for early detection of any suspicious changes in the skin.
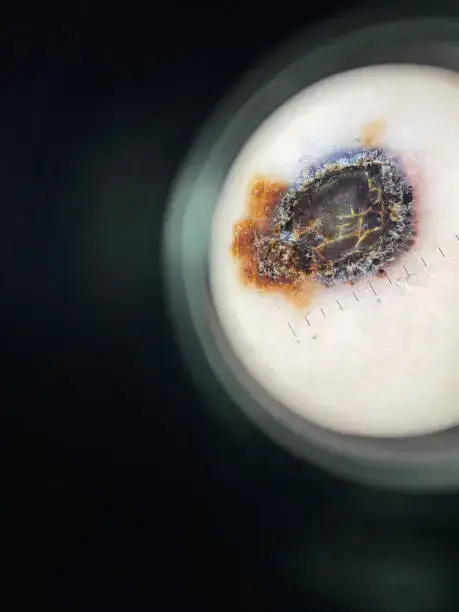
During a physical examination, the dermatologist examines the patient’s skin meticulously for any irregular moles or lesions. They assess the characteristics of existing moles based on the ABCDE criteria: Asymmetry, Border irregularity, Color variation, Diameter larger than 6 mm, and Evolution over time. This initial assessment is essential, as it helps in recognizing potential early signs of melanoma.
Following the physical examination, dermatoscopy may be employed. This technique utilizes a specialized light source and magnification to allow the dermatologist to visualize skin lesions in greater detail. Dermatoscopy is an invaluable tool that can help differentiate between benign and malignant growths, providing a clearer understanding of the lesion’s structure and composition. This non-invasive technique greatly enhances the accuracy of melanoma diagnosis.
Ultimately, if a suspicious mole or lesion is identified, a biopsy is conducted. This procedure involves removing a sample of the tissue for laboratory analysis. There are various biopsy techniques available, including excisional, incisional, and punch biopsies, each chosen based on the characteristics of the lesion and the surrounding skin. The biopsy results are critical, as they confirm the presence of melanoma and determine its specific type and stage, guiding subsequent treatment options.
In conclusion, the diagnosis of melanoma is a multi-faceted process that highlights the importance of early detection through regular skin examinations. By understanding the methods employed in the diagnostic process, individuals can take proactive measures in their skin health, ultimately leading to better outcomes in melanoma treatment.
Stages of Melanoma
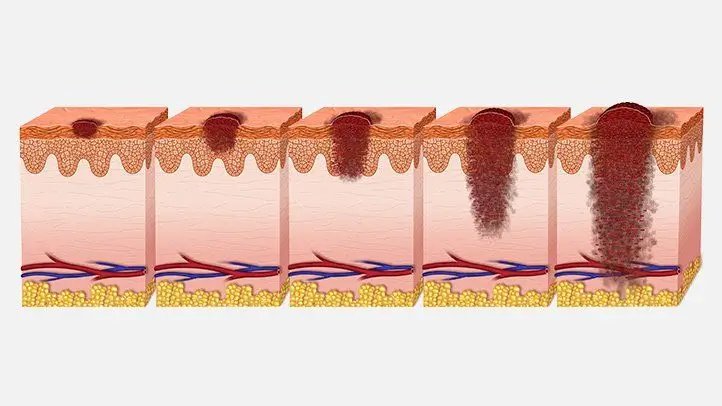
Melanoma is classified into several stages based on the extent of the disease, which ranges from stage 0, known as in situ melanoma, to stage IV, where the cancer has metastasized to distant sites. Understanding these stages is crucial for determining appropriate treatment options and predicting patient outcomes.
Stage 0 indicates that the melanoma is confined to the outer layer of skin, or epidermis. At this stage, the cancerous cells have not invaded deeper layers of the skin, which results in a high prognosis for complete recovery with early treatment. Common treatments for stage 0 melanoma include surgical excision, where the melanoma is completely removed, ensuring minimal risk of spread.
In stage I, the melanoma has grown deeper into the skin but remains localized. This stage can be divided into IA and IB, depending on the thickness and whether the cancer has ulcerated. The prognosis remains favorable, with treatment usually involving surgical removal of the tumor, often supplemented by sentinel lymph node biopsy to check for any microscopic spread.
Stage II melanoma is characterized by further thickness and ulceration, indicating a greater risk of spread. Similar to stage I, treatment primarily revolves around surgical intervention, but may also include discussions of adjuvant therapies, particularly for high-risk patients.
Stage III signifies regional spread, where the melanoma has reached nearby lymph nodes. This stage presents more complexity in treatment decisions, potentially incorporating surgery, targeted therapies, or immunotherapy to address cancer cells that may have escaped the primary site.
Finally, stage IV is recognized as advanced melanoma, having metastasized to distant organs such as the lungs, liver, or brain. The prognosis at this stage is less favorable; however, numerous treatment options exist, including systemic therapies and clinical trials, aimed at managing the disease and prolonging survival.
Treatment Options for Melanoma
Melanoma, a serious form of skin cancer, often necessitates a comprehensive and personalized approach to treatment. The selection of treatment options largely hinges on the stage of melanoma, as well as individual patient characteristics such as age, overall health, and personal preferences. Surgical intervention is frequently the primary treatment for localized melanoma, involving the excision of the tumor along with a margin of healthy tissue to ensure complete removal. In cases where the melanoma has progressed, further treatment modalities become essential.
Immunotherapy has emerged as a vital option for advanced melanoma. This approach boosts the body’s immune response against cancer cells and can be particularly effective in cases where melanoma has metastasized. Common immunotherapy agents include checkpoint inhibitors such as pembrolizumab and nivolumab. These medications work by unleashing the immune system’s ability to destroy cancer cells, offering new hope for patients with limited options.
Targeted therapy represents another vital treatment strategy, specifically aimed at melanoma patients with certain genetic mutations, such as BRAF mutations. Targeted therapies like vemurafenib and dabrafenib aim to inhibit the growth of cancer cells by blocking the specific pathways that the tumors rely on for survival. On the other hand, traditional chemotherapy has seen a decline in use for mela-noma due to the advent of more effective treatments like immunotherapy and targeted therapy; however, it may still be employed in certain situations, particularly aggressive or unresponsive cases.
Lastly, radiation therapy could be utilized in various contexts, such as alleviating symptoms from metastatic mela-noma or as an adjunct to surgery when dealing with high-risk lesions. Combining treatments, such as utilizing radiation alongside surgery or immunotherapy, can also be a strategic approach to optimizing outcomes. Given the complex nature of mela-noma, it is essential for healthcare providers to tailor treatment plans to each patient, ensuring the best possible prognosis and quality of life.
Preventive Measures and Skin Care

Preventive measures play a crucial role in reducing the risk of mela-noma skin cancer. One of the most effective strategies is the consistent use of broad-spectrum sunscreen with an SPF of at least 30. This should be applied generously to all exposed skin and reapplied every two hours, or more frequently after swimming or sweating. The protective benefit of sunscreen cannot be overstated, as it acts as a barrier against harmful ultraviolet (UV) rays that contribute to skin damage and increase the likelihood of developing mela-noma.
In addition to sunscreen, wearing protective clothing is essential when spending extended periods outdoors. Long-sleeved shirts, wide-brimmed hats, and UV-blocking sunglasses are excellent choices. These garments not only shield the skin from harmful rays but also help to maintain overall skin health. Reduced exposure to the sun during peak hours, specifically between 10 a.m. and 4 p.m., is another key preventive measure. Seeking shade during these hours can significantly decrease sun exposure and lower the risk of skin cancer.
Regular skin checks and self-examinations should be an indispensable part of personal skin care. Individuals are encouraged to inspect their skin monthly for any new or changing moles, lesions, or spots. The ABCDE rule is a helpful guideline: look for asymmetry, irregular borders, varied colors, a diameter larger than 6mm, and any evolution in size, shape, or color. Early detection of changes can lead to prompt medical attention and potentially successful treatment outcomes.
Incorporating these preventive strategies into daily routines not only enhances skin protection but promotes a proactive approach towards skin health. By understanding and applying these measures, individuals can significantly decrease their risk of mela-noma and ensure early detection when necessary.
Living with Melanoma: Support and Resources
Receiving a diagnosis of mela-noma can evoke a range of emotional and psychological challenges for individuals and their families. It is essential for patients to acknowledge these feelings, as they may experience anxiety, fear, or depression due to the uncertainties associated with cancer treatment. Coping with the complexities of mela-noma not only affects the patient but also their loved ones who may share in the distress. Therefore, it becomes vital to create a robust support system during this challenging time.
Support can come in various forms, from healthcare professionals, family, and friends to support groups and online resources. Engaging with healthcare teams ensures that patients receive not only medical treatment but also emotional care. Oncologists, nurses, and social workers are available to provide comprehensive support and address any concerns patients may have regarding their condition and treatment modalities. These professionals can guide patients through the complexities of managing their disease while encouraging them to communicate openly about their feelings.
Support groups can play a crucial role in fostering a sense of community among individuals dealing with mela-noma. Many organizations focus on cancer support and offer both in-person and virtual support groups where patients can share experiences, challenges, and coping strategies. The connection with others facing similar obstacles can be incredibly validating and comforting, thus alleviating feelings of isolation. Additionally, several resources are available through charities and non-profit organizations tailored specifically to melanoma. These groups may provide educational materials, financial assistance, and access to clinical trials, further empowering patients and their families.
Ultimately, understanding and utilizing available support and resources can significantly enhance the quality of life for individuals living with mela-noma. By fostering connections and seeking help when needed, patients can navigate their journey with greater resilience and hope.
Conclusion and Future Directions in Melanoma Research
In summary, understanding mela-noma skin cancer is paramount for effective diagnosis, treatment, and prevention. This form of skin cancer poses significant health risks, particularly for individuals with fair skin, a history of sun exposure, or a family history of the disease. The symptoms can vary, but early detection remains crucial for improving patient outcomes. Effective awareness of such symptoms allows for prompt medical attention, potentially leading to better prognoses.
Recent advancements in mela-noma treatment have introduced a range of innovative therapies, including immunotherapy and targeted therapy, which have significantly improved survival rates for advanced mela-noma cases. Ongoing research into these emerging treatments is vital, as it aims to enhance their efficacy and reduce side effects, ultimately providing more tailored options for patients. Furthermore, the development of combination therapies shows promise in overcoming resistance to treatments and improving overall efficacy.
In addition to advancements in treatment, the field is witnessing a concerted effort towards developing better diagnostic tools. Enhanced imaging techniques and biomarker studies may lead to earlier detection of mela-noma, further improving treatment outcomes. Research is also focusing on understanding the genetic and molecular basis of mela-noma, which could unlock new therapeutic targets and strategies.
As scientists and healthcare providers continue to explore the intricacies of mela-noma, it is vital for patients and the general public to remain informed about the latest research findings. Active participation in discussions about skin health, risk factors, and treatments can foster a community better equipped to combat mela-noma. Thus, staying engaged with ongoing advancements will play a key role in the future direction of mela-noma research and formulating effective prevention strategies.
Did You Try this tips ?
There are no reviews yet. Be the first one to write one.
blood work brain health climate health diabetes treatments digestive health disease management disease mapping exercise plan fitness tips hair care hair growth hair treatment headache treatment health care health expenses health foods health insurance health secrets health tips healthy alternatives healthy habits healthy recipes heart health home workouts immune boost immune foods keto delivery lifestyle diseases medicine innovation mental health morning exercise natural remedies nutritional advice raw nutrition skin cancer skin care skin health sleep exercise sleep technology telemedicine services telemedicine solutions unhealthy habits viral threats walking benefits weight loss